Healthcare Payer Solutions
Healthcare Payers face many challenges in the healthcare industry, from expanding regulations to improving the member and provider experience. Demands are high and disruption is everywhere. Kiriworks is focused on helping payers meet the increased expectations for both service and compliance. Our solutions touch multiple departments, such as Appeals & Grievances, Network Operations, Member Services, Compliance, Back Office and IT. Built on the industry-leading content services platform by Hyland, our solutions help drive accelerated performance and innovation to meet the demands of this dynamic industry.
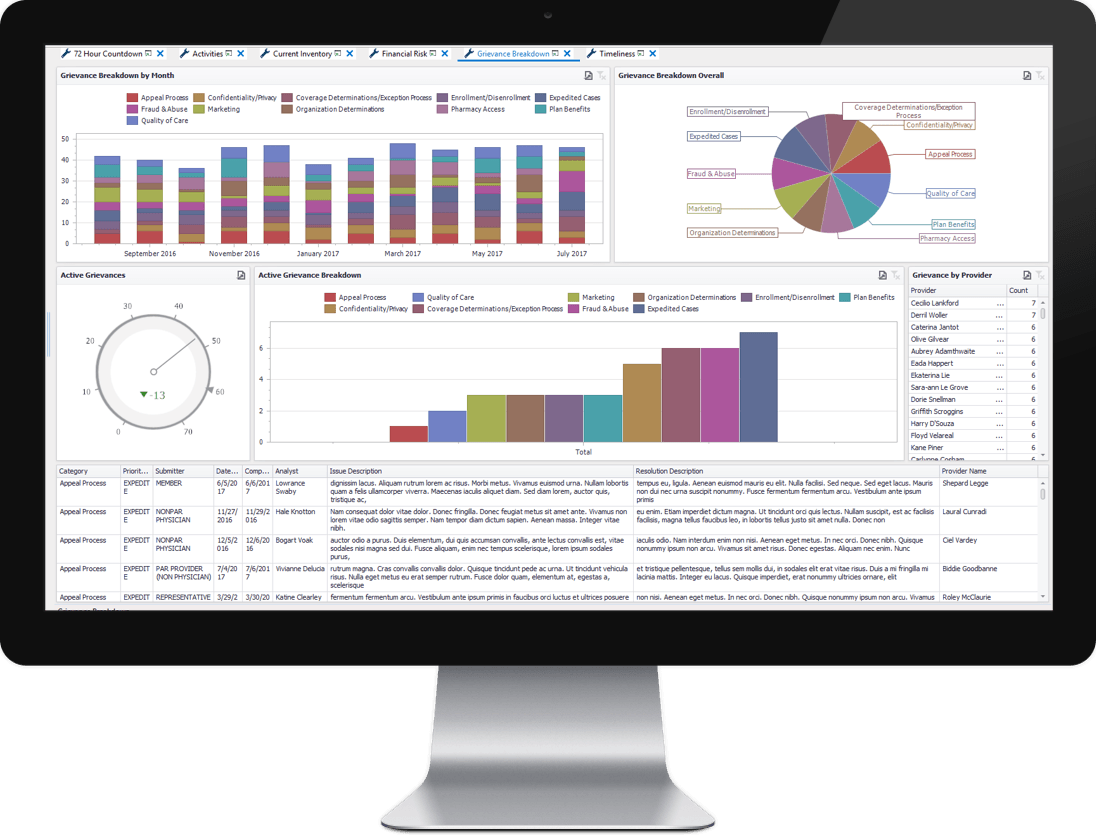
Appeals & Grievances
Kiriworks A&G manages every aspect of the appeals and grievances process. From Medicare, Medicaid and Commercial plans - Kiriworks A&G has been designed with compliance at the center of the solution. Kiriworks A&G starts managing and monitoring the process the second an appeal, grievance, compliant or inquiry is received. From automated correspondence creation, IRE packet generation, CDAG & ODAG universe reporting, data validation reporting and real-time process dashboards - Kiriworks A&G has you covered.
Learn More
Organization Determinations
As an extension of the Kiriworks A&G for Medicare solution accelerator, Kiriworks Organization Determinations brings the same holistic, case management approach to managing a healthcare payer's organization or initial determinations. Kiriworks Organization Determinations manages the request from intake through resolution with auto-calculated due dates, system-generated notifications and a portfolio of management and regulatory reports.
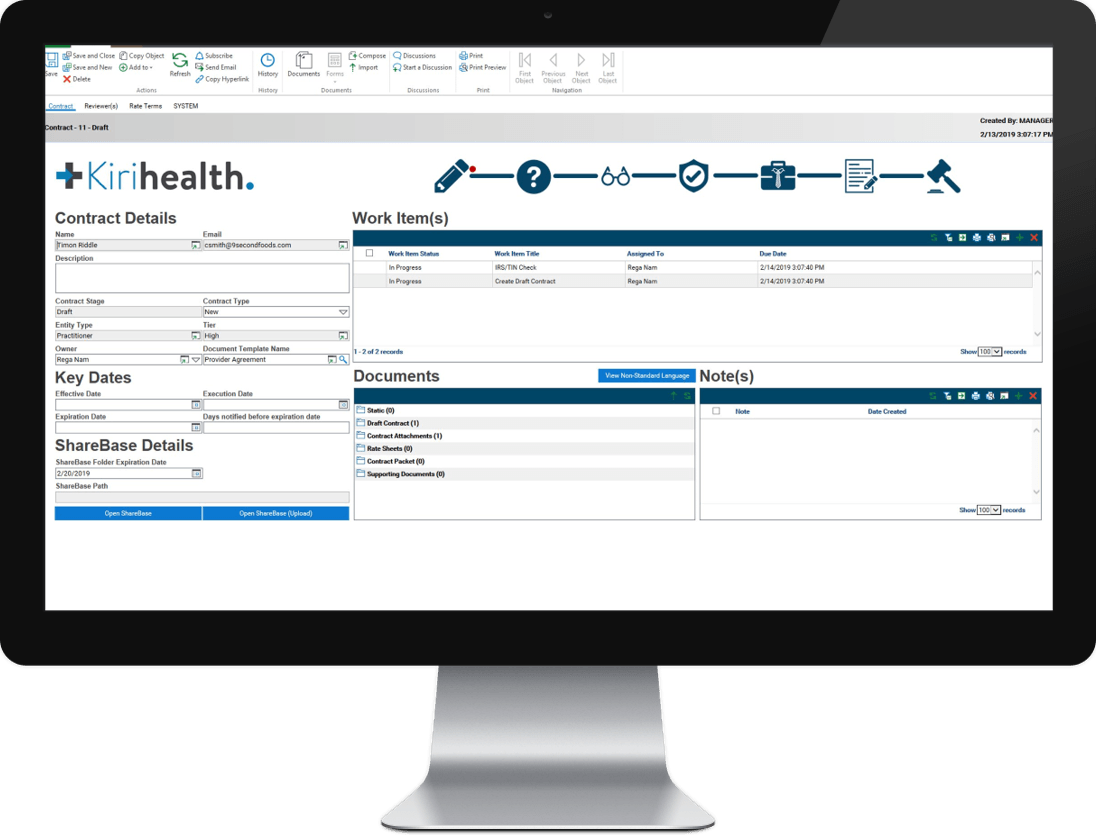
Network Development & Contracting
Kiriworks Network Development & Contracting is designed to create a collaborative approach to the provider contracting process. With integrated workflow automation and content services, Kiriworks Network Development & Contracting automates and manages the process from provider recruitment to contract management (creation, negotiation and execution) through provider onboarding and renewal/termination management.
Learn More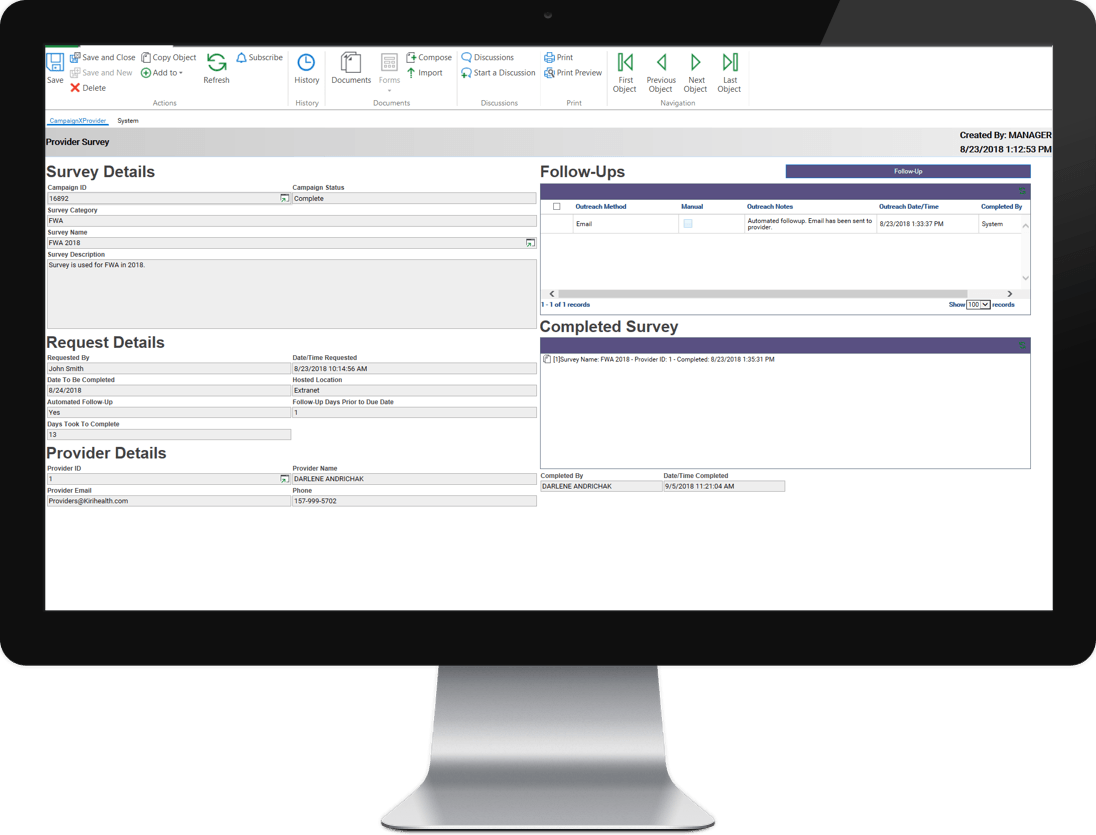
Provider Outreach
Kiriworks Provider Outreach is a platform designed to manage the outreach and analyze the responses of a healthcare payers provider network. Kiriworks Provider Outreach is used to design, distribute, manage and report on all aspects of your provider outreach program. Whether you are sending attestations, surveys, questionnaires or friendly reminders, Kiriworks Provider Outreach is a way to bridge the communication gap between your provider network.
Learn More
Provider Credentialing
Part of the Kiriworks Provider Management Platform, Kiriworks Provider Credentialing enables healthcare payers to digitally transform their credentialing process. Kiriworks Provider Credentialing can be used by healthcare payers as a stand along application or connected to the Kiriworks Network Development & Contracting solution accelerator. Kiriworks Provider Credentialing guides users through the credentialing process with configurable activities based upon regulations, policies and state requirements.
Provider Site Surveys
Another component of the Kiriworks Provider Management Platform is Kiriworks Provider Site Surveys. Whether a site survey is triggered during the provider contracting process or based upon a grievance related to a member's experience with a provider - Kiriworks Provider Site Surveys delivers healthcare payers a complete mobile survey experience that is directly connected to their provider data and the case that initiated the site visit. Users have the ability to conduct their site visit from a mobile device while capturing video and photo and completing the required questionnaires.
Content Connect
Content Connect leverages a healthcare payer's existing secure infrastructure and services to digitally route the right information to the right person at the right time. Content Connect enables payers and providers to share data and documents in seconds, not days, while eliminating lost or misplaced information. By ensuring authorized users have immediate access to accurate, up-to-date data and documents, Content Connect facilitates improved communication with both payers and providers.
Learn MoreDISCLAIMER: While Kiriworks healthcare payer accelerator products are designed to aid in the collection, management and reporting of business content, these products do not relieve users of responsibility to insure compliance with all applicable state and federal regulations and implement procedures to examine and verify for completeness and accuracy of all data and output before its use.